Do Varicose Veins Run in Families?

Varicose veins 一 a common condition notorious for causing enlarged, twisted veins 一 affect as many as 35% of Americans.
If someone in your family has varicose veins, you might wonder whether varicose veins run in families and if there is a genetic predisposition to developing this condition.
Below, Dr. Henock Saint-Jacques and our team here at Harlem Cardiology explore the connection between varicose veins and genetics, shedding light on the factors that contribute to their development and what you can do to manage and prevent them.
The genetic influence on varicose veins
There are a few ways that your genetics can affect your vascular health. This includes:
Family history
Research suggests that there is indeed a genetic component to varicose veins. If you have a family member, particularly a parent or sibling, who has experienced varicose veins, you may be at a higher risk of developing them as well. Studies have shown that individuals with a positive family history are more likely to develop varicose veins compared to those without a familial predisposition.
Inherited weakness of vein walls and valves
The structure and function of veins play a significant role in the development of varicose veins. In some cases, individuals inherit weaker vein walls and valves, making their veins more prone to stretching and becoming insufficient. When the valves fail to efficiently regulate blood flow and prevent backflow, it can lead to the pooling of blood, resulting in the formation of varicose veins.
Genetic factors that influence your vein health
Various genetic factors contribute to the development of varicose veins. For instance, certain genes involved in the regulation of collagen and elastin, which are crucial components of vein walls, can impact their strength and elasticity.
Genetic variations associated with inflammation and blood clotting processes may also play a role in the development of varicose veins.
Mutations on the FOXC2 gene are associated with an increased risk of lymphedema, which can also increase your risk of developing varicose veins.
Managing and preventing varicose veins:
While you may have a genetic predisposition to varicose veins, there are steps you can take to manage and prevent their occurrence:
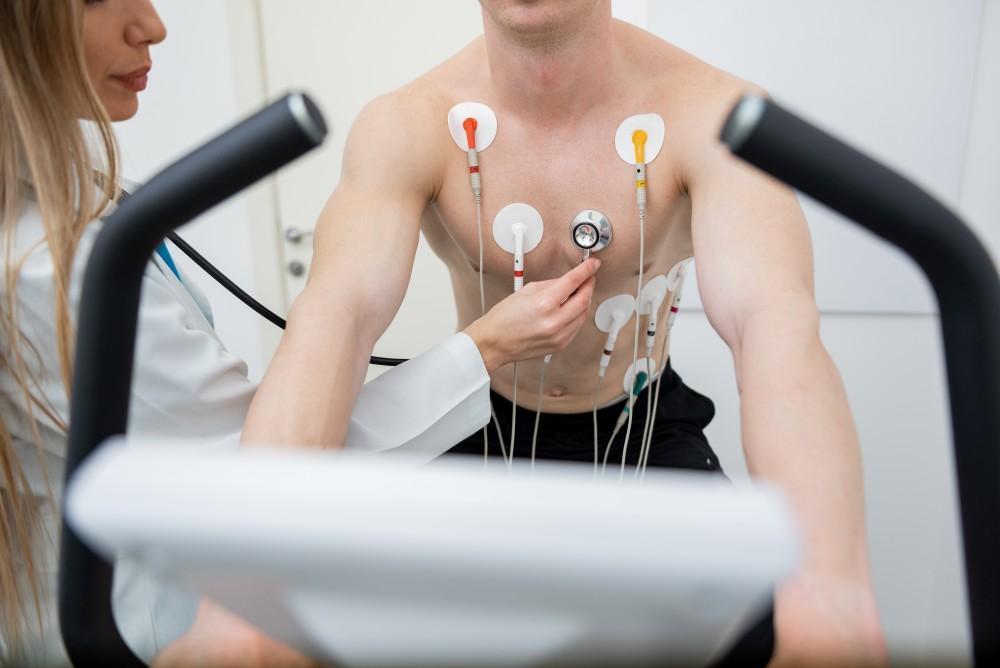
Regular exercise
Engaging in regular physical activity, particularly exercises that promote leg strength and circulation, can help reduce your risk of varicose veins. Activities such as walking, cycling, and swimming can improve blood flow and strengthen the muscles that support healthy vein function.
Maintain a healthy weight
Maintaining a healthy weight can help alleviate pressure on your veins and reduce the risk of developing varicose veins. Excess weight puts additional strain on your legs and can impair proper blood circulation, contributing to the formation of varicose veins.
Avoid prolonged standing or sitting
Avoid long periods of standing or sitting in one position, as it can lead to poor circulation and increased pressure on your veins. If your job requires prolonged periods of sitting or standing, take regular breaks to move around and stretch your legs.
Elevate legs and wear compression stockings
Elevating your legs above the heart level whenever possible can help promote better blood flow and relieve pressure on the veins. Additionally, wearing compression stockings or socks can provide support to the veins and assist in maintaining proper circulation.
Seek medical treatment
If you’re already experiencing varicose veins or related symptoms, don’t hesitate to reach out. Varicose veins are often regarded as a cosmetic issue, but the reality is that they cause uncomfortable cramping or aches, and they can also be a warning sign of vascular issues, such as chronic venous insufficiency.
Here at Harlem Cardiology, Dr. Saint-Jacques can recommend appropriate treatment options, such as sclerotherapy, laser therapy, radiofrequency ablation, high ligation and vein stripping, ambulatory phlebectomy, or endoscopic procedures, to manage and improve the appearance of your varicose veins.
To explore your treatment options, schedule your varicose vein consultation with Dr. Saint-Jacques at 646-381-2181 or through our online form.
You Might Also Enjoy...

Is It Possible to Lower My Blood Pressure Naturally or Do I Need Medicine?

What You Can Do Now to Prevent a Stroke Later in Life

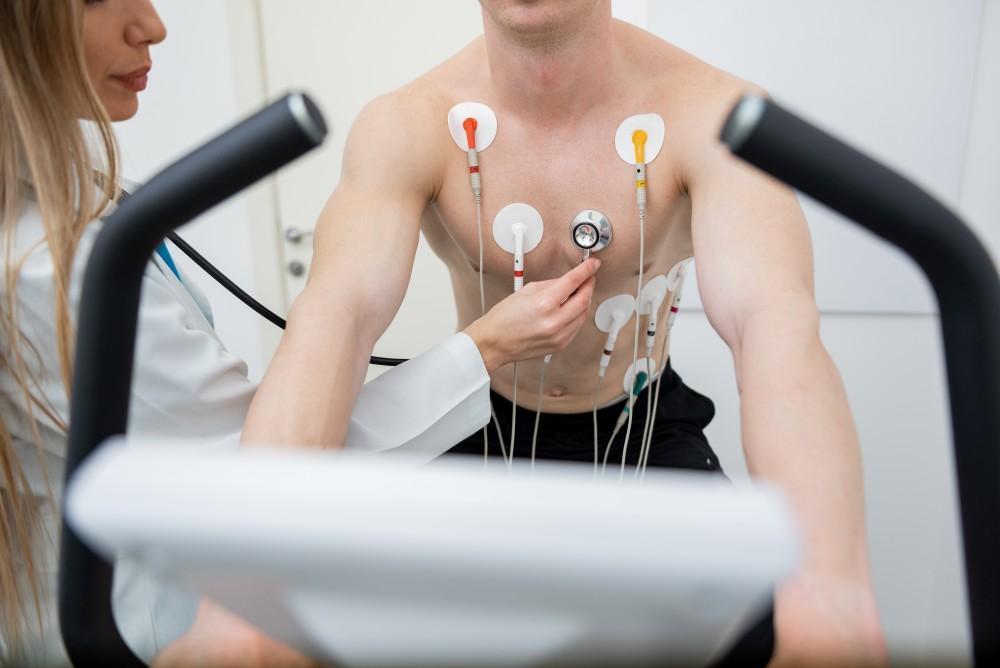
3 Noninvasive Tests That Measure the Health of Your Heart

What Can I Do About My Varicose Veins?


